The Role of AI in Ethical Decision-Making for Implantable Devices
Table of Contents
- Why AI is Entering the Ethics Conversation in Cardiology
- Ethical Dimensions at the Intersection of AI and Implantables
- Accountability and Clinical Governance
- India’s Unique Position: A Chance to Build Responsible Innovation from the Ground Up
- Final Thoughts
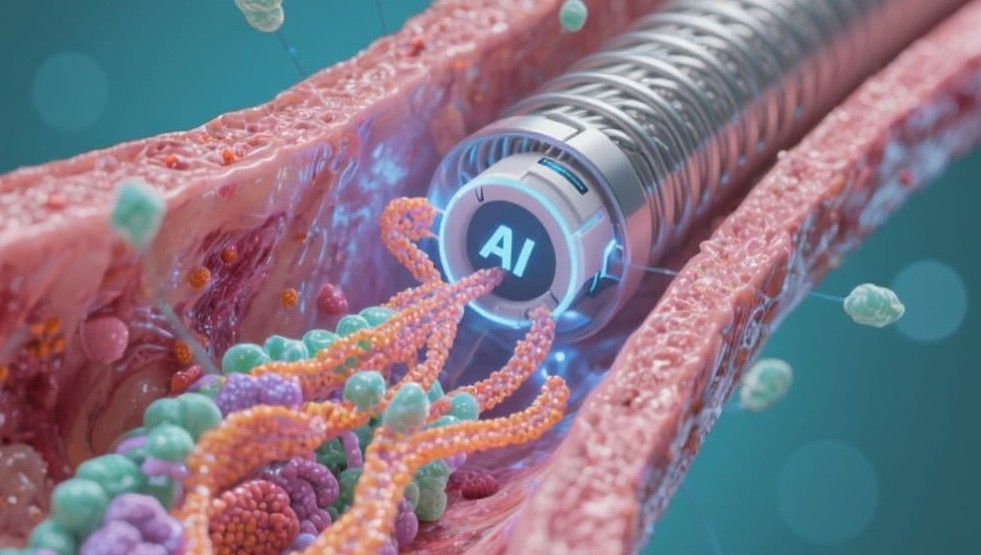
As artificial intelligence (AI) becomes increasingly embedded in healthcare, its role in the design, deployment, and management of implantable cardiac devices is drawing significant attention—not just for its technical promise but for the ethical implications it carries.
Cardiac implantables such as pacemakers, ICDs, and drug-eluting stents with embedded sensors are evolving from static hardware to intelligent systems that collect, interpret, and act on real-time data. This shift raises a critical question:
Who makes the decisions when machines start interpreting health signals that were once the sole domain of human clinicians?
In a country like India—where cardiac disease is rampant, healthcare infrastructure is uneven, and access to specialists is limited—this question becomes even more pertinent.
Why AI is Entering the Ethics Conversation in Cardiology
AI’s applications in cardiovascular care are far-reaching:
- Predictive analytics for restenosis post-stenting
- Autonomous pacing adjustments in pacemakers
- Personalized device programming based on continuous learning models
- Triage and intervention recommendation systems linked to implantable telemetry
These systems are trained on massive datasets, including ECGs, imaging, EHRs, and even behavioral data. The AI doesn’t just assist physicians—it can sometimes override clinical defaults or prompt autonomous actions.
This is where ethics enters the picture.
Ethical Dimensions at the Intersection of AI and Implantables
1. Informed Consent and Transparency
Patients receiving implantable devices often don’t fully understand what data is being collected, how it will be used, or by whom.
In India, a study by AIIMS and ICMR found that only 28% of cardiac patients receiving AI-integrated implants were aware of the device's data-sharing capabilities.
Transparency becomes crucial when AI recommendations influence life-altering decisions such as pacing thresholds, defibrillation triggers, or dosage adjustments.
Ethical AI mandates that patients be told not just what the device does, but how its algorithms make decisions, and what control the clinician retains.
2. Bias and Data Representation
AI systems are only as good as the data they’re trained on. Most AI models used in implantable device R&D are trained on Western patient datasets, which may not reflect Indian anatomical, genetic, or lifestyle nuances.
This mismatch can result in:
- Incorrect risk stratification
- Device malperformance
- Over- or under-treatment in Indian populations
To be ethically viable in India, these systems must be trained on diverse, local datasets. The government’s Ayushman Bharat Digital Mission (ABDM), which is building a national health data ecosystem, may play a pivotal role in enabling this.
3. Autonomy vs. Algorithm
What happens when an AI-driven implant recommends something that contradicts the judgment of a trained cardiologist—or vice versa?
- Should an ICD autonomously deliver a shock based on a false positive from an AI reading?
- If an AI recommends device explantation based on usage patterns, who takes responsibility?
In ethical AI frameworks, human override must remain a key feature. The European Union’s AI Act and the US FDA’s Good Machine Learning Practice (GMLP) emphasize that AI should augment, not replace, clinician decision-making. India’s regulatory ecosystem is still evolving in this regard, but CDSCO has indicated interest in adopting AI governance norms in alignment with these global trends.
4. Data Privacy and Security
Implantable devices collect highly sensitive health data in real time. As AI models run edge or cloud-based analytics on this data, issues around data encryption, storage jurisdiction, and third-party access arise.
- The Digital Personal Data Protection Act, 2023 in India mandates that personal health data be stored securely and only used with clear, revocable consent.
- MedTech developers must integrate privacy-by-design principles, ensuring that patient data used in training or real-time AI applications is anonymized, encrypted, and non-commercially exploited.
Any deviation risks eroding public trust in both the device and the system.
5. Accountability and Clinical Governance
If an AI-enabled implant fails—or causes harm—who is accountable? The manufacturer? The algorithm developer? The clinician? The hospital?
This “black box” problem has prompted the global MedTech community to develop audit trails, decision logs, and fail-safes that can trace back how a decision was made. For ethical deployment in India, the same must be locally mandated through Medical Device Rules (MDR) updates and industry-led governance.
India’s Unique Position: A Chance to Build Responsible Innovation from the Ground Up
India is not just adopting AI in implantable devices—it’s building them. Startups, R&D labs, and global players in India are developing AI-driven pacing systems, diagnostic catheters, and smart stents tailored to Indian patient needs.
This puts India in a rare position to embed ethical principles from the design stage, rather than retrofitting them later. By:
- Training AI on inclusive, local datasets
- Designing for consent-first use cases
- Ensuring human-centered algorithm transparency
India can lead not just in affordable innovation, but in responsible and ethical innovation.
Final Thoughts
AI is becoming a silent but powerful actor in cardiovascular care. For implantable devices, this raises profound ethical considerations that can no longer be treated as afterthoughts.
India has both the technical talent and the regulatory momentum to build AI systems that are not just smart, but safe, inclusive, and ethically sound. The future of cardiac care depends not only on how intelligent our devices become, but on how responsibly we allow them to decide.
